Health Information
COMMON EQUINE DISEASES & CONCERNS
We have compiled summaries for some of the most common and concerning diseases that affect horses in the UK. This is designed to give a broad overview of what to look out for and treatment plans that we might offer. Please always call us if you have concerns about your horse’s health. We are here to help 24/7.

Equine Emergency
At South Moor Equine we believe you should have access to the best veterinary care for your horses, whatever the time of day. That is why we provide a 24-hour, 365-day, out of hours service for when an equine emergency occurs, staffed by our own vets with access to all our mobile equipment.
Whilst we hope no owner ever has to call us in an emergency situation, should you need to speak to one of our vets you can call any of our numbers which will put you through to one of our on call nurses. They can arrange for a vet to call you, or to attend to your horse directly.
The most important thing to do in an emergency situation is to stay calm, and keep yourself safe. You should never jeopardise your own safety, your horse needs you uninjured to make sure they get the best help possible. If it is possible and safe to do so, move the horse to a safe environment where he or she can be controlled for the vet to fully examine, e.g. a stable or yard.
Excessive bleeding can be controlled by placing firm pressure on the wound with a non-stick material. Again it is important to remember that even the calmest horse can react unpredictably when they are in pain or stressed. Ideally do not give any medications before seeking the vet’s advice, but if you do ensure you let the vet know what you have given, and at what time.
Whilst we can deal with the majority of veterinary issues at your yard or field, we also have good relationships with the local referral hospitals. So should your horse need further specialist or surgical care, we can refer him or her to a referral hospital for further treatment.
If you want advice on if your horse needs to be seen, or what to do whilst waiting for the vets to arrive, we are always happy to call first to discuss the case.

Atypical Myopathy (AM)
There has recently been a number of cases of Atypical Myopathy (AM) diagnosed in the UK and subsequently a lot of information in the press and online. We have collated a summary of the latest research and information regarding this disease.
What is Atypical Myopathy?
It is a disease that occurs in horses which can be potentially fatal. It is also know as Sycamore Poisoning in the UK due to this particular type of tree being at the heart of the disease. Trees of the Maple family including Sycamores contain a toxin in the leaves and seeds that fall from the tree which can be ingested during grazing.
There is still a lot about this disease which is not fully understood and much research is ongoing. Outbreaks of atypical myopathy (AM) largely occur in Autumn and it has been strongly linked to a toxin (called hypoglycin A) within the leaves and seeds of the maple family.
Unfortunately for us in the UK, Sycamore tress fall into this family. We do get other members of the Maple family in this country as well such as the Box Elder but they are not native. Sycamore trees are obviously very common but it is very difficult to predict the risk to your horses even if they are grazing in a field surrounded by Sycamores. This is because the amount of toxin in the leaves and seeds varies between trees and also between seeds/leaves of an individual tree. The chance of your horse getting AM, therefore, seems to depend on the amount of seeds/leaves they ingest as well as the concentration of toxin that is in those seeds/leaves they have ingested.
What are the risk factors for Atypical Myopathy?
- Strong winds often precede outbreaks as more leaves/seeds are blown onto pasture.
- Affected horses obviously need to be grazing.
- Autumn time.
Atypical Myopathy (AM) is highly fatal but about a quarter of cases survive. This means that the sooner the vet is called once you recognise there is a problem, the faster AM can be diagnosed and the faster it can be treated; improving the chance of survival.
AM affects multiple organ systems, so can cause varying symptoms and makes them truly intensive care patients. The more mild the symptoms, the better the prognosis. Reduced exposure to sycamore seeds/leaves will reduce the risk, either by removing them from pasture if possible or restricting grazing to unaffected areas.
Symptoms include:
- Weakness
- Pain
- Stiffness
- Tremors
- Recumbency
- Respiratory difficulty
- Prevention
Don’t panic!
Remember there are numerous examples of horses co-existing with maple species and having no problems. However, increased awareness will hopefully lead to better prevention and horses receiving treatment sooner.

Sweet Itch
What is Sweet Itch?
Sweet Itch is an allergic skin condition in horses due to the saliva of biting midges. This is usually more common in the UK during the warmer months. The protein molecules within the midges saliva causes an immune response or reaction on the skin of the horse. This reaction can vary between individual horses and naturally there is a varying range of treatments. The best treatment is preventative action, however should you have any concerns you should always make contact with an equine specialist veterinarian.

Advice for sweet itch management:
- Confirm the nature of your horse’s skin complaint. There are a large number of causes of equine skin diseases, such as fungal (ringworm), bacterial (rainscald), parasitic (lice, mange), as well as allergic reactions to bedding, insect bites, dust mites and pollens. If you are in doubt or need help to diagnose your horses condition please call the team at South Moor Equine for further advice 01548 830210.
- Use insect repellents or insecticidal sprays such as Switch or Deosect regularly to reduce attack from biting insects. These contain permethrin, making them very effective, and can be bought from the practice.
- Use a fly sheet to help avoid contact with the biting insects. Ones with attached head masks and belly protection can be useful in more affected horses.
- Install a fan in the stable – midges can’t fly in wind speeds over 5mph.
- Apply a fly screen to the stable door and windows.
- Use topical oils to discourage midges and black flies from landing on the skin and feeding many people swear by the original formula Avon Skin So Soft, (which will also help protect you from those pesky horse flies).
- Move your horse to a windy hillside where biting insects tend to avoid.
- Don’t keep your horse near watercourses and trees, where there are high numbers of biting insects.
- Stable your horse at dawn and dusk when it is open to attack from biting insects.
- Only rely on corticosteroids as a last result because of the risk of setting off laminitis.

Strangles
What is strangles?
Strangles is caused by a bacteria called Streptococcus equi. It is a common, highly contagious infection of a horse’s upper respiratory tract. It can cause large abscesses to form, make swallowing difficult, restrict breathing and be both painful and distressing for the horse.
Persistent infection can develop that results in horses becoming long-term strangles carriers
Redwings Horse Snctuary have put together a comprehensive review on the disease, which we would recommend all our Equine Clients to read.

Equine Gastric Ulceration Syndrome
What is Equine Gastric Ulceration Syndrome (EGUS)?
It is a condition in horses which causes depreciated performance and colic. Ulcers are formed in the horses stomach which lead to pain, dietary issues and clear changes in the horses typical behaviour and performance.
Symptoms of Equine Gastric Ulceration Syndrome include:
- Recurrent colic
- Weight loss
- Poor appetite
- Coat changes
- Poor performance
- Behavioural changes
- Discomfort when girthing
Diagnosis:
Gastroscopy is the only accurate was to diagnose EGUS. This is done under standing sedation at your own yard using our portable video system. A camera is passed up the horse’s nose and down to the stomach. Horses must be starved for 16 hours prior to examination and have water removed 1-2 hours before we start.

Kissing Spine
What is Equine Kissing Spine?
Kissing spine (Overriding/Impinging Dorsal Spinous Processes) occurs when the spinous processes of the vertebrae touch or rub together and is likely to cause pain and discomfort for your horse.
Why does kissing spine happen?
There is several theories, but it is not strictly understood. It is likely to be multifactorial. A weakness in the back leads to a dip, which sets off a cycle of pain. To better understand the condition we need to first understand the horses anatomy:
- Each vertebrae in the horse’s back has 2 transverse processes and a dorsal process (one on each side pointing outwards=transverse, and one on top pointing upwards=dorsal).
- Each dorsal spinous process (DSP) is buried in the epaxial muscles which run down each side of the back on the left and right of midline, above each transverse process and to each side of the DSP.
- Each DSP is linked above by the supraspinous ligament which runs along the top of them all. In between each adjacent DSP is the interspinous ligament which gets compressed and stretched as they move.
Kissing Spines Symptoms:
- Poor performance
- Poor jumping
- Breaking stride (especially downhill)
- Back pain
- Behavioural problems
- Resistance to tacking
- Rearing/ bucking
- Lameness (chicken and egg)
- Vague and variable!
- Symptoms similar to some other conditions!
Impinging (Kissing) DSPs
- There are 18 thoracic and 6 lumbar vertebrae.
- The most common sites for kissing spines are betweenT11 and T13, but they can occur anywhere between T10 and L6.
- Kissing spines therefore cause thoracolumbar pain.
- T11-T13 is the saddle region
Diagnosis
- Manual palpation: This is subjective, but an experienced equine vet should have a good appreciation for what is ‘normal’ or abnormal. Palpation cannot diagnose kissing spines alone! It is important on the day of the vet visit that the horse has not already been exercised and hasn’t done any extremely strenuous exercise in the last couple of days.
- Radiography (x-rays): Vital part of diagnosis and with modern digital x-ray equipment we can get very good diagnostic x-rays of horse’s backs in practice. Radiographically we see reduction of the interspinous space, sometimes overlapping DSPs and often bone changes on the DSPs. But studies show that radiography alone is probably not enough on which to base a diagnosis, because some clinically normal horses will have radiographic changes.
- Scintigraphy (Bone Scan): Can be useful to diagnose kissing spines in combination with x-rays.
- Local anaesthetic block
- Response to medication
Treatment
- Physio: Secondary muscle pain is a big part of this condition and an equine physio can help reduce this and help build core strength to support the back.
- Medication: We can inject the offending spaces to reduce pain and inflammation.
- Surgery: Interspinous Ligament Desmotomy is minimally invasive and has good outcomes. DSP resection is possible in some cases.
- Possible treatments and management options would be discussed with the veterinary surgeon depending on individual circumstances.

Foal Heat Diarrhoea
What is Foal Heat Diarrhoea?
Foal Heat Diarrhoea is the name given for the short periods of diarrhoea often seen in foals aged 5 to 14 days old who are otherwise fit and healthy. It is seen in 80-95% of normal foals, with no breed pre-disposition.
What causes Foal Heat Diarrhoea?
Originally it was called ‘Heat Diarrhoea’ as if often occurs at the same time as the dam’s first return to oestrus, and was thought to be caused by a change in hormones in the mother’s milk. However, new studies have failed to make an association between foal heat in the mare and the onset of diarrhoea in foals. Furthermore, it is often seen in orphan foals and those fed on milk replacer! The most recent theory suggests it’s a natural change in the foal’s natural gut flora that causes the diarrhoea, particularly as the foal begins to ingest other feeds.
What does it look like?
Foals will remain bright, sucking well and have a normal temperature. The diarrhoea is mildly loose and watery but often malodorous, but will clear up within 3-7 days. Hair loss and scalding of the perineal area is commonly seen.
How can I treat Foal Heat Diarrhoea?
Treatment is usually unnecessary as the diarrhoea is self-limiting. However, as with all diarrhoea it is important to keep the perineum clean and dry and prevent scalding over the hindquarters by using petroleum jelly or similar. We can provide supplements to help foals with diarrhoea which we usually have in stock and can be supplied without examination of the foal. If you are concerned, just give us a call!
When should I call the vet?
Prognosis for Foal Heat Diarrhoea is very good, however any foal with diarrhoea needs to be closely monitored as foals with diarrhoea can deteriorate rapidly. If the foal goes off colour, the diarrhoea is prolonged or you notice any other symptoms please get in touch with us ASAP.

Lameness
What is Horse Lameness?
Lameness is a common problem in equine veterinary care. It refers to the unusual stance of a horse that is caused by an issue with the horses locomotor system. This is usually due to pain but can also be a neurological issue or wider faults in the mechanical makeup of the horse. A Lame horse will usually show signs of the condition such as a limp and obvious bobbing of the head. Quick diagnosis is vital. South Moor Equine Vets are able to diagnose and treat causes of horse lameness such as foot abscesses and tendon injuries as well as perform thorough investigations and treatments.
What may a horse lameness work up include?
- Taking a thorough history of the horse
- Testing for pain in the horses hoof
- Careful examination of your horses conformation
- Palpation of your horses limbs and back
- Active lameness assessment at walk, trot on different surfaces, lunging, and flexion tests or even being ridden
- Relevant diagnostic imaging including x-ray or ultrasound
- Nerve or Joint blocks (injections)
- Referral for specialist diagnostic imaging such as an MRI scan or scintigraphy
If it is unclear what the cause of horse lameness is, one or a series of nerve blocks may be performed: a small volume of local anaesthetic is injected, over specific nerves in the leg to numb the feeling to a specific area of the horse. If your horse/pony is sound after this nerve block then we know that the cause of lameness is coming from somewhere within the ‘blocked’ region. If your horse/pony remains lame then we will perform the next nerve block up the leg.
What happens after a lameness work-up?
We would always discuss the outcome of a lameness work-up with you before undergoing any treatment. The type of treatment is very dependent on the diagnosis but may include: Medication of a structure with an anti-inflammatory drug e.g. placing steroid into a joint, rest +/- controlled exercise, changes to the way your horse is shod, systemic treatment with an anti-inflammatory (e.g. ‘Bute’), surgery to treat specific conditions and/or to provide us with more diagnostic information.

Pre-Purchase Exams
What is Horse Lameness?
Lameness is a common problem in equine veterinary care. It refers to the unusual stance of a horse that is caused by an issue with the horses locomotor system. This is usually due to pain but can also be a neurological issue or wider faults in the mechanical makeup of the horse. A Lame horse will usually show signs of the condition such as a limp and obvious bobbing of the head. Quick diagnosis is vital. South Moor Equine Vets are able to diagnose and treat causes of horse lameness such as foot abscesses and tendon injuries as well as perform thorough investigations and treatments.
What may a horse lameness work up include?
- Taking a thorough history of the horse
- Testing for pain in the horses hoof
- Careful examination of your horses conformation
- Palpation of your horses limbs and back
- Active lameness assessment at walk, trot on different surfaces, lunging, and flexion tests or even being ridden
- Relevant diagnostic imaging including x-ray or ultrasound
- Nerve or Joint blocks (injections)
- Referral for specialist diagnostic imaging such as an MRI scan or scintigraphy
If it is unclear what the cause of horse lameness is, one or a series of nerve blocks may be performed: a small volume of local anaesthetic is injected, over specific nerves in the leg to numb the feeling to a specific area of the horse. If your horse/pony is sound after this nerve block then we know that the cause of lameness is coming from somewhere within the ‘blocked’ region. If your horse/pony remains lame then we will perform the next nerve block up the leg.
What happens after a lameness work-up?
We would always discuss the outcome of a lameness work-up with you before undergoing any treatment. The type of treatment is very dependent on the diagnosis but may include: Medication of a structure with an anti-inflammatory drug e.g. placing steroid into a joint, rest +/- controlled exercise, changes to the way your horse is shod, systemic treatment with an anti-inflammatory (e.g. ‘Bute’), surgery to treat specific conditions and/or to provide us with more diagnostic information.

Equine Flu Vaccinations
There are many different horse governing bodies across the UK depending on the discipline. Although equine flu is endemic in the UK, we periodically get outbreaks, which are taken very seriously. For up-to-date information on the state of equine flu in the UK currently go to https://equinesurveillance.org. British Equestrian is a useful source of up-to-date vaccination guidance: https://www.britishequestrian.org.uk/
This is a guide to help you understand what vaccines your horse needs and when. It is correct at the time of writing, but please check with your own governing body to ensure full compliance with the latest rules.
Although different bodies allow different vaccination time intervals, we strongly recommend following the manufacturer’s instructions:
- Two vaccinations 4-6 weeks apart (primary course; from 5 months of age).
- 3rd vaccination 5 months after the 2nd.
- Booster vaccinations every 6 months to 1 year (depending on your situation and governing body rules you compete under).
Please remember that vaccinations are the responsibility of the owner of the horse and not the veterinary practice! We do our best to provide timely and accurate vaccination reminders, but very occasionally contact details are incorrect or something goes wrong and reminders are not received, but we cannot be held responsible for an owner not remembering their horse’s vaccinations!
The guidance below was last updated in June 2025
- First two vaccinations 21-60 days apart (primary course)
- 3rd vaccination 120-180 days after the 2nd.
- Booster no more than 6 months apart.
Horses that go over 6 months on their booster must re-start the course.
Horse that were up to date with flu vaccinations prior to January 2022 can just continue on the 6-monthly boosters and do not need to re-start. Any horse starting a vaccination course from January 2022 must comply with the new rules.
Horses cannot race within 7 days of a previous vaccination (day of vaccine is day 1) and must have received the first two vaccinations before racing.
FEI
All flu vaccinations must now be recorded in FEI horse app by your veterinarian. Please ensure you have your passport available at the time of vaccination.
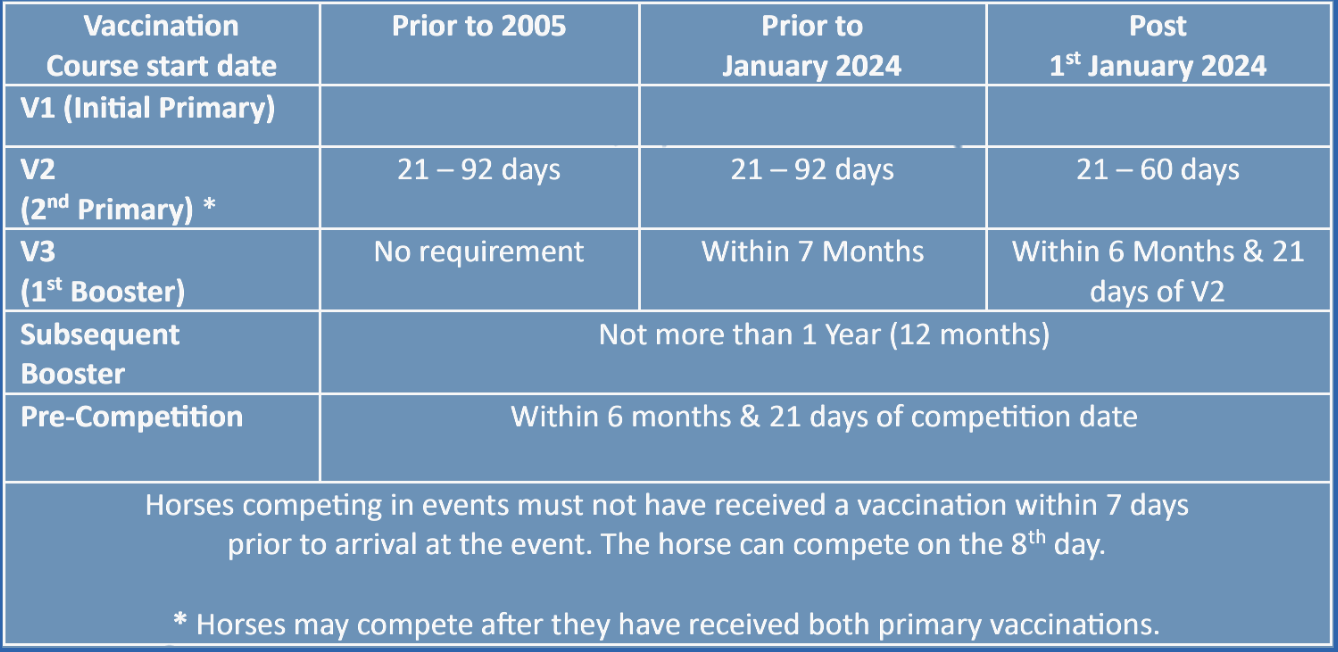
Horses who had their primary course of vaccinations prior to January 2024 do not need to restart.
British Eventing – Primary Course as per FEI, Boosters within 12 months
British Dressage – Primary Course as per FEI, Boosters within 12 months
British Showjumping – Primary Course as per FEI, Boosters within 12 months
Pony Club – Primary Course as per FEI, Boosters within 12 months (6 monthly vaccination is recommended)
British Riding Club – Primary Course as per FEI, Boosters within 12 months (6 monthly vaccination is recommended)
DO NOT LET YOUR HORSE’S VACCINATIONS GO OVER 365 DAYS OR YOU WILL NEED TO RESTART.

Castration
Castrating (or ‘cutting’) your colt or stallion can be a daunting prospect, but is usually the best decision for the horse to enable him to live with other horses. If the horse is not going to be used for breeding, castration is usually advised.
Why Castrate a Horse?
- Prevent unwanted stallion-like behaviour
- Can improve behaviour towards people
- Reduces fighting
- Reduces mounting of other horses
It must be remembered that if stallions are castrated later in life some of this behaviour will be ‘learned’ and castration will not abolish it.
When To Castrate?
We can castrate a horse at any age, but recommend it being done after 5-6 months. This is usually when they start to show some colt-type behaviour and the testicles are still quite small, therefore so are the blood vessels reducing risk of bleeding. Some people prefer to leave them until they are a bit older due to perceived benefits with respect to growth and development. Timing will depend on your aspirations for the horse, experience and facilities available.
What Are Possible Complications of Castrating a Horse?
- Swelling: some swelling is to be expected post-surgery. If you are concerned about how much it is best to call for advice.
- Infection: Infection is a risk with any surgical procedure. Usually it is because the incision has closed early, before drainage has resolved.
- Bleeding: This is a risk in the immediate post-operative period. ‘Open’ castrations (no ligatures) are expected to bleed, but as a general rule of thumb, if you can’t count the drips because it is too fast you need to call the vet. Bloody-coloured fluid can drain from open castration incisions for several days intermittently.
- Eventration: This is a rare but potentially very serious complication where a portion of gut has descended through the inguinal canal and out of the surgical site. If you see anything sausage-like protruding after castration it is an emergency and a vet is required. Rarely, a piece of omentum (lacy-looking tissue) can protrude: this is less serious but still needs seeing by a vet as an emergency.
How To Provide Post-operative Care For a Castrated Horse?
The vet will tell you about how to care for the horse after surgery. As a guide, we recommend the horse is kept in a stable and quiet that night, before being turned out the following day onto a paddock which isn’t too muddy. It is important the horse gets some exercise daily, so if he is not moving around in the paddock then a lead walk twice daily would be advised.
The vet will probably provide you with oral medication to be given twice daily for a period following surgery. But, don’t panic, although it is a surgical procedure and risks/complications are possible, it is very routine for us and complications are fortunately rare.
What happens?
In a nutshell both testicles and their associated structures are removed surgically. We have two basic options for equine castrations: recumbent (anaesthetised; ‘knocked out’) or standing.
Standing Castration:
- No anaesthetic risk (done under sedation and local anaesthetic)
- No risk from induction/recovery
- Cheaper
- Can’t be done in miniatures or small hairy ponies as not enough room!
- No sutures are placed and haemostasis (prevention of bleeding) relies on clots in blood vessels as a result of the emasculators (surgical clamping tool) used.
- Can take longer to fully heal and can drain for many days.
Recumbent Castration:
- Can be done exactly the same as standing but under anaesthesia.
- Ligatures can be placed (under very clean conditions) reducing risk of bleeding and other complications.
- Suitable place required: with lots of room if any larger than a miniature.
- If outside very weather dependent on the day
- More expensive
- Some increased risks, mostly associated with induction and recovery from anaesthesia.
The exact surgical method used will depend on the vet and their personal preferences and previous experience.

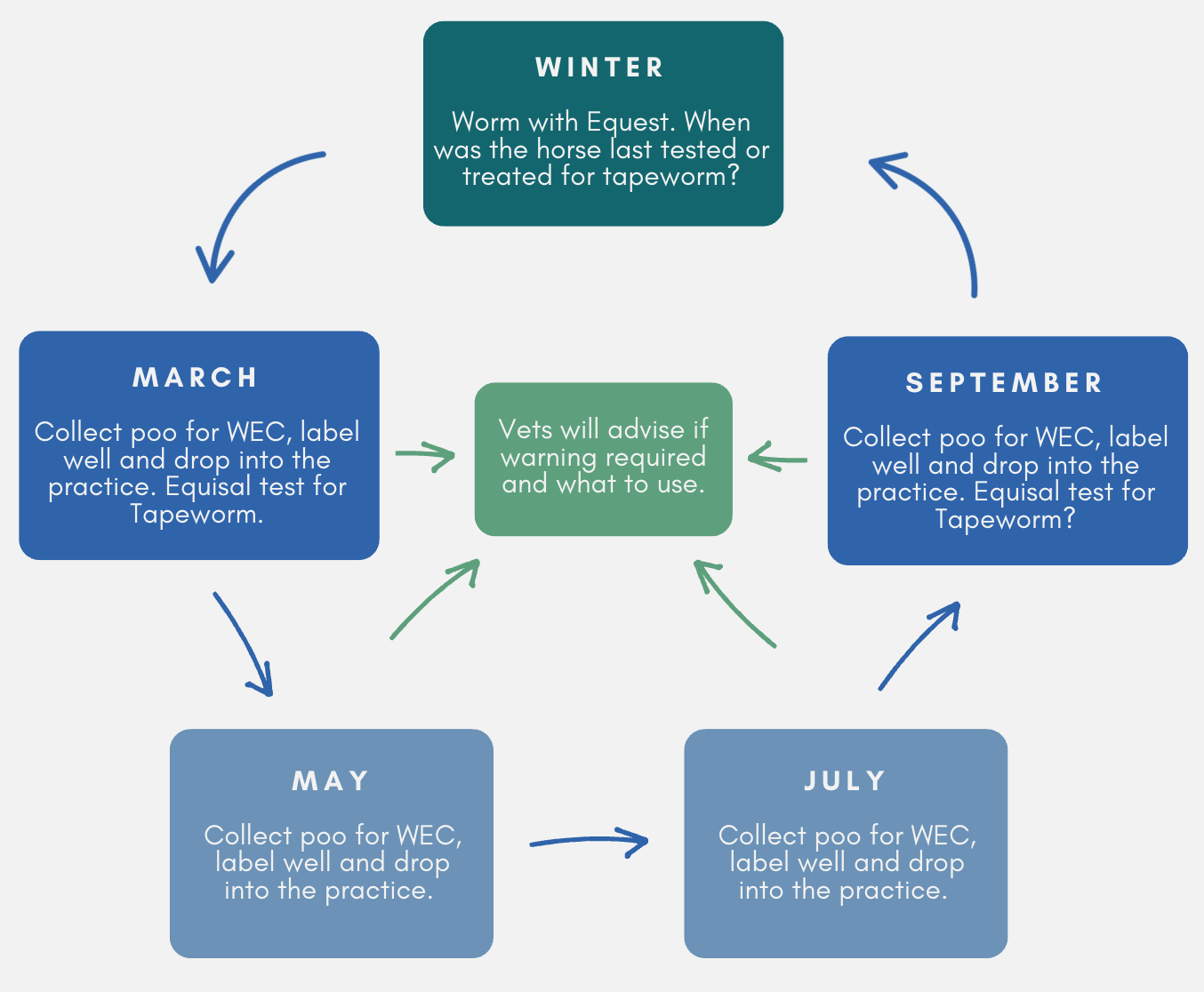
Equine Worming Guide
Horse worming schedule throughout the year:
(this may vary between yards depending on various factors)
Horse Worming
Resistance to equine wormers is a problem that affects us all and is likely to become an ever more serious issue in the future. Resistance is promoted every time a wormer is used, as some of the worms in a horse are likely to be naturally resistant to the wormer. Thus, when the wormer is used, the sensitive ones are killed and resistant ones left behind to multiply on your fields. Over time, there is significant risk that this resistant population will build up and result in wide-spread wormer resistance across the UK. This issue is important if you just keep one horse or are on a big livery yard. Resistance to cyathostomins (small redworm) has been reported in all types of wormers.
Young Horses
Youngsters (less than 18 months) are more at risk of high worm burdens as their immunity has not developed fully yet, so we need to be more careful with this age group.. Please contact us for specific advice from one of our vets about worm management in youngsters.
Worm Egg Counts (WECs)
To avoid the spread of resistance we strongly recommend the use of WECs to detect which horses actually need worming. 80% of horses do not need worming during the Spring and Summer months. WECs are not useful over winter months as the small redworm encyst in the gut wall inside the horse and are therefore not producing eggs detectable in the poo. We recommend WECs are done every 2-3 months from March to October depending on risk and history. If a horse has a very high WEC result, we may recommend repeating the WEC 2 weeks after worming to ensure it has been effective.
How to collect poo for WEC
Collect a sample from fresh poo passed within the previous 12 hours. Take small amounts from several different parts of the pile to make a sample which is about a handful in total. Mix it up, place it all in a sealable bag and expel the air before posting/dropping it at one of our branches as soon as you can.
Tapeworm
High burdens of tapeworm are relatively uncommon but can cause serious colic when present in large numbers. Traditionally horses have been treated for tapeworm twice a year, but again, this risks development of resistance over time. We now recommend the use of the Equisal saliva test for tapeworm once or twice a year, so we only treat horses that have high numbers present. Equisal tests can be ordered from our practice, come with instructions and are performed by yourself. We will then report the result back to you and advise on any treatment necessary.

Equine Herpes Virus (EHV)
The two most important equine herpes viruses are EHV-1 and EHV-4. These viruses usually cause respiratory disease, but can cause neurological disease and abortion. EHV-1 is much more commonly associated with neurological disease and abortion than EHV-4. Most horses in the UK have probably been affected by this virus at some point in their lives and can harbour ‘latent’ virus, which can then start shedding at times of stress, making it impossible to eradicate this disease.
Symptoms
- Respiratory – can be very mild
- Cough
- Nasal discharge
- Off colour
- High temperature (easily missed as can go up and down)
- Inappetence and lethargy
Abortion
- Usually in mares after 5 months.
- High temperature (easily missed as can go up and down)
- ‘Red bag’ delivery
- No warning signs
- Can also cause death of new-born foals
Neurological
- Variable severity: mild hind limb weakness to completely unable to stand.
- High temperature (easily missed as can go up and down)
- Inappetence and lethargy
Diagnosis
The vet will take 2 samples from a horse suspected to have EHV. One is special swab taken from up the nose and into the horse’s throat and the other is a blood sample. A second blood sample will be required 2 weeks after the first in most cases.
Prevention
Complete prevention is impossible as most horses carry latent (and undetectable) virus that can start shedding at any time. But the risk can be significantly reduced by the following:
- New arrivals onto a yard should be isolated from the others for 3 weeks and have their temperatures taken twice daily. They could also receive an EHV vaccine booster prior to relocation.
- Walk-in mares and new arrivals on studs should be kept separate to resident mares and in-foal mares. Mares coming in to foal should arrive at least 28 days before foaling.
- Young stock (<2yo) should be kept separate to in-foal mares.
- Minimise stress as much as possible e.g. maintain small established social groups as much as possible and make changes slowly.
- Because EHV cannot be prevented there is no point ‘blacklisting’ horses that have been previously diagnosed (all horses are likely to have latent virus). But isolation of new arrivals reduces the risk of spreading of EHV from shedding horses that are stressed from moving home.
Outbreak
If a case is suspected, it should be isolated from the others immediately and the vet called. Stringent biosecurity measures should be put in place until the lab results have come back or until the vet says it is ok to relax them. Horses that have been in contact with the affected horse should be isolated from all others in a further group and monitored very closely with twice daily temperature monitoring. All movement on and off the yard needs to be stopped. Virucidal disinfectants, PPE and biosecurity barriers are required. Further information on this would be provided by the vet at the time and/or can be found on the Equibiosafe app (free to download) and on the HBLB codes of practice.
Vaccination
Vaccination of your horse will not prevent EHV but it will reduce the risk and reduce severity. Pregnant mares should be vaccinated at 5, 7 and 9 months of gestation and all others should have a primary course 4 weeks apart followed by a booster every 6 months. There are no requirements for EHV vaccination currently in the UK, but it is recommended that competition horses and racehorses are vaccinated due to increased stress, higher risk of coming into contact with unknown horses and the negative effect on performance that would be seen with respiratory disease.
All horses on a yard/premises with pregnant mares should be vaccinated against EHV.